There are so many questions that come up when I am asked about TMS, the most often being: “What the heck is that?”
TMS stands for Transcranial Magnetic Stimulation. This is a fancy way of saying we use electromagnetic energy to wake up the brain. Think of it like jumpstarting a car- but the car is your brain, and instead of using direct electricity we use MRI technology. This is possible by applying Faraday’s Law, which states that any magnetic field produces an electric field and vice versa.
Here are the top 10 most commonly asked questions I get when asked about my job and what exactly it entails.
How does it work?
As you may already know, the brain is made up of neurons (nerve cells) that are composed of chemical energy which in turn produces electrical energy to power the rest of your body.
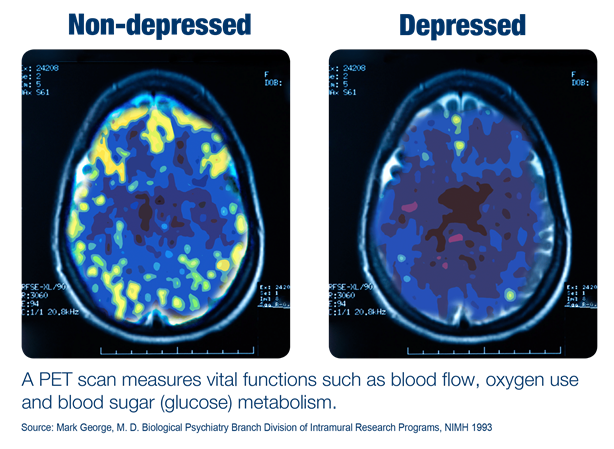
Generally speaking, people who suffer from depression have less overall activity in the brain than non-depressed people do (see Image 1)
TMS utilizes MRI technology to “wake up” these neurons. For those who have never received an MRI, it is a harmless and painless procedure used to display soft tissues in the brain by orienting the atoms in neurons in a way that allows us to view the electrical activity.
The area targeted during TMS for treatment of depression is the dorsolateral prefrontal cortex (yes, I know, it is a mouthful). Dorso- (like the dorsal fin of a shark) means the top of your head, lateral meaning the side, and prefrontal meaning the area just before your frontal cortex. So essentially, the area just above your left temple. Scientists have chosen this area because it is connected to other parts of the brain associated with mood management. Among these parts include the amygdala which processes the feelings of emotions, the hippocampus which stores memories (as most people with depression suffer from a decrease in memory functioning), and the anterior cingulate cortex which controls our responses to emotionally relevant information.
 Does it hurt?
Does it hurt?
While TMS does not necessarily feel pleasant most people would describe it as generally “annoying” or mildly uncomfortable. The first week of treatment tends to be the most difficult as we start at a low level of energy and gradually increase the necessary amount of energy to the ideal level. After this period of adjustment, patients tend to tolerate the treatment much easier. You cannot feel it on your brain nor below the skull as our brains do not have pain receptors directly on them. There is some irritation around the scalp where the coil is placed as most people feel a strong tapping or a “wood-pecker” like feeling. If there is any sort of intolerable discomfort that may arise during treatment your TMS technician is specially trained to make minor adjustments to the location of the coil to a more comfortable position under the supervision of the doctor on site.
Who can benefit from TMS?
TMS is most often associated with treating depression. However, it can be used for a plethora of other disorders such as anxiety, OCD, addiction, PTSD, or even Multiple Sclerosis. The protocol
varies for each, as they are all specially designed to isolate specific areas depending on the condition. At our office, we offer precise protocols for depression, anxiety, OCD, and PTSD.
What are the side effects?
Compared to most medications, the amount of side effects is incredibly minimal. The most common one reported, however, is headaches. Though these tend to go away after the first two to three weeks for most people, patients are advised to take ibuprofen or other over-the-counter painkillers as needed.
Others describe experiencing fatigue during the day. As the second most common side effect, it can potentially have an impact on one’s day-to-day activities. Patients are encouraged to rest as needed and to do their best to get a good night of sleep between treatments as poor sleep can negatively impact the outcome of treatments.
It is also crucial to mention that the side effects vary from person to person, and side effects may last longer or shorter depending on many things. For example, the amount of energy required, how depressed a patient might be, certain pre-existing health conditions, or consumption of alcohol or marijuana intake. Though, it is important to note that we usually skip treatments when a patient has been drinking or using other mind-altering substances as it can have varying side effects and impact the overall outcome of treatments.
How effective is it?
Research suggests TMS is about 70% to 80% effective with around half of patients not needing to return for maintenance sessions afterward. From my own experience, I would say this is accurate – about 75% of the patients I have seen make a significant recovery – with only a handful of them returning for sessions after about a year or two. The schedule for said maintenance sessions varies for each patient depending on need.
(You can find this information as well as more details about efficacy at https://www.tmsbrainhealth.com/tms-therapy/what-is-the-success-rate-of-tms-therapy/)
How much does it cost?
Most insurances cover TMS, with the out-of-pocket cost often equivalent to the copay for a regular doctor’s office visit. Treatments are about 20 minutes each, 5 days a week for 6 weeks, plus three additional weeks of staggered treatments for the patient to taper off. This equals a total of 36 sessions. As an example, if your normal copay is $20 for a visit to an office, you would pay about $720 (that’s 36 days times $20). If you are interested in treatment, we advise reaching out to your insurance company to see what the cost would be, as deductibles and
out-of-pocket maximums vary from patient to patient.
One of the most common concerns from patients is the commitment of coming in every single day in combination with the side effects.
I like to remind patients that they are in a period of crucial treatment. In the same way that a person with Crohn’s disease receives Remicade, or a person with cancer receives chemotherapy, this is a life-changing and life-saving treatment that should be taken as such. We often have patients who are career-oriented or family-oriented. We fully support patients to
continue focusing on the things they love and the passions that fuel their daily lives. Still, we encourage patients to take this treatment to heart as much as they can to make the most out of it.
Though accommodations may be available for a patient through FMLA or a letter from the doctor, we strongly encourage patients to first communicate with their work, school, or family to make adjustments to their schedule as needed.
How do I know if it is working?
One of the first signs I look to see if the treatment is working is an improvement in sleep and the presence of vivid dreams. During sleep, our brains are actually more active than when we are awake. This is why the odd phenomenon is called Paradoxical Sleep. Thus, experiencing intense dreams is a display of overall increased activity. People also describe an increase in energy levels throughout the day, feeling more patient or less agitated, and sometimes even an increase or decrease in appetite (depending on the person’s baseline depressive symptoms relative to food intake).
What happens during treatment?
After the first session where the doctor is present, each patient is assigned a technician. Patients are welcome to choose a technician who they believe may be a good fit for them (check out your options on our website for bios on our available technicians!). Each patient is placed with the same technician every day. This is so the progress of the patient can be tracked consistently, and appropriate adjustments required during treatment can be made based on that person’s unique needs. Generally speaking, we often see that patients are most comfortable when they are familiar with the person assisting them. In my own experience, I have developed close relationships with patients in the same way a consistent therapist might.
Many of our patients enjoy listening to music, podcasts, or even playing games on their phone during treatment (and no, the machine will not make your phone blow up). On the other hand, many like to spend their time chatting with their technician about… pretty much anything and everything! The choice is up to you. And don’t worry – we won’t be offended if you prefer to sit back and relax with earbuds in!
Does the doctor give the treatment?
The doctor is present for the first initial mapping. This is a procedure in which we use the machine to find where the prefrontal cortex is specific to you. It is painless, and most patients describe the feeling of a light tapping on their heads if they do feel anything at all. Following the mapping, you are placed with a trained and certified TMS Technician that will assist you for the remainder of treatments. The doctor will be on-site, however, so she can assist you with any concerns that may come up. Another wonder of TMS is that each treatment is specially designed for each patient. The location of the prefrontal cortex is different for each person as well as the energy level required. No two patients are exactly alike (even if you are twins!).
What is a “Mapping”?
(My favorite part!) This happens during your first treatment. It only takes about 1 to 2 hours to complete. The doctor and the designated technician will use the machine to send a series of electromagnetic signals to your brain to find your area. But how does it do that?
The brain, as complex as we perceive it to be, is designed very simply. We first target an area that we refer to as the motor cortex, which is essentially a strip of neurons stretching from the left side of your brain to the right. Imagine if you are wearing a headband stretching from ear to ear, across the top of your head. At a point in the middle of the headband, there is a tiny clump of neurons associated with the muscles in your leg. Hypothetically, if we were to send an electromagnetic pulse to this area, we would see a slight and painless twitch in your leg. If you keep moving down the headband along the side, getting closer to your ear, we will find your arm muscles, hand muscles, and then facial muscles – consecutively (see the Image 2). We stay in the area just near your hand as we send very subtle signals to this area to look for tiny movements in your thumb. We isolate the location of the thumb because it is precisely 5.5 cm behind the mood area we aim to target. Therefore, after finding the location of the thumb, we move forward that equal distance and apply the treatments to the uniquely located prefrontal cortex.
While the above covers the basics of treatments, more than likely it will spark further interest and even more questions about TMS. Thus, we welcome you to give our office a call Monday through Friday 9:00 AM to 5:00 PM, or feel free to stop by our location in Vancouver, Washington to meet our staff and ask all the questions you like!
Author